Darla’s story: From stroke to hospital to rehabilitative therapy
In January of 2024, Darla Black was visiting her daughter’s home in Spokane to attend her grandson’s basketball tournament. On Sunday morning, she awoke to find she had trouble moving her right arm. Several months previously, she’d had a transient ischemic attack (TIA), a brief stroke-like attack, so she immediately recognized what was happening: she’d had a stroke during the night.
But the TIA wasn’t her only clue. As a retired nurse with a 46-year career providing inpatient rehabilitation care in Great Falls, Montana to patients with a variety of conditions, she was acutely in tune with her symptoms.
“I sat up on the bed and couldn’t move my right side at all,” Darla said. “My right hand worked just a little, but otherwise nothing. So I called for my daughter and told her we needed to get to a hospital right away.”
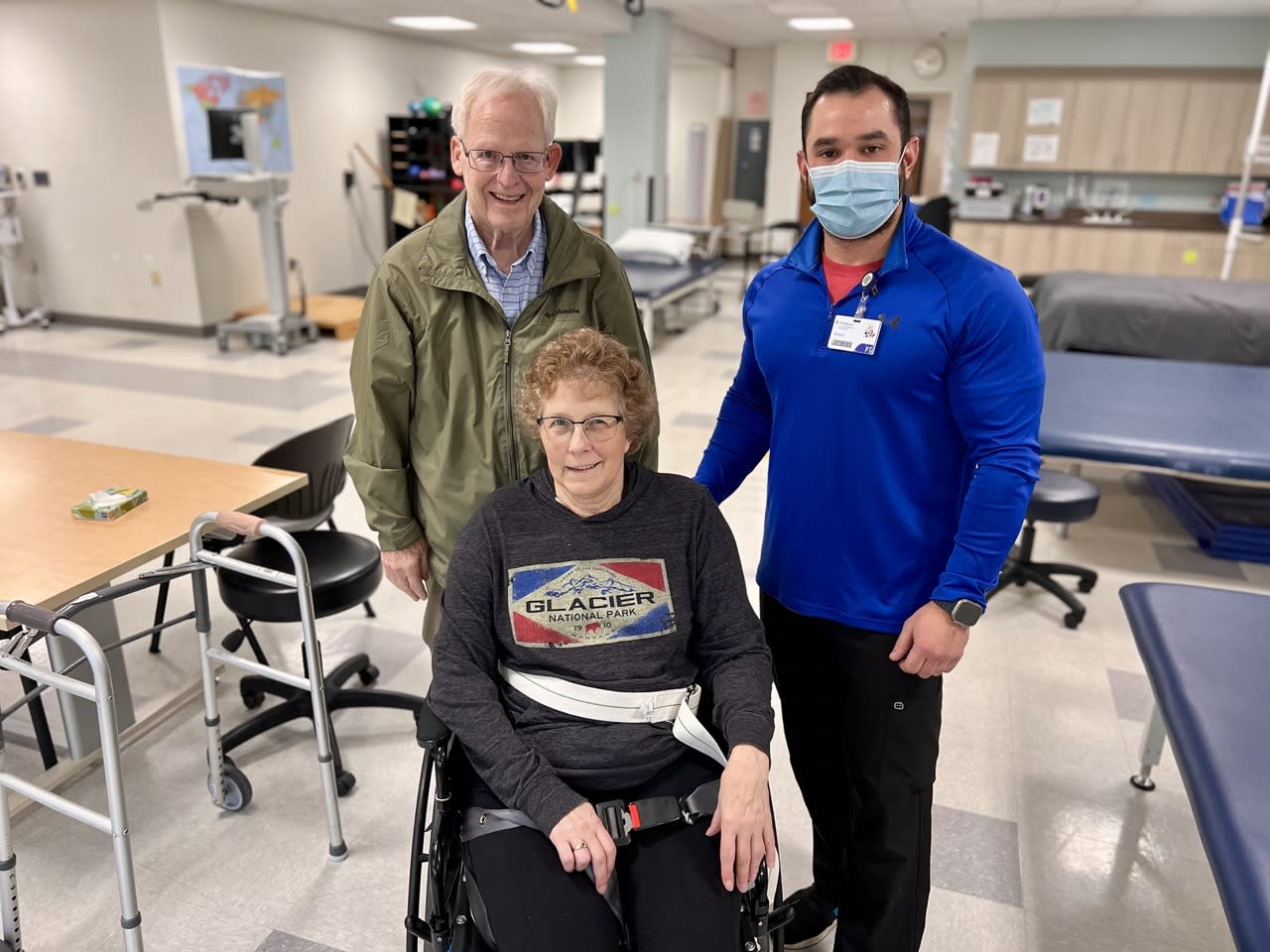
Darla spent three days as an inpatient receiving blood thinning medication and was closely observed by doctors who helped stem the impact of the event. Following that, like any stroke patient, Darla needed ongoing rehabilitation to help restore her quality of life. Whereas many care facilities limit rehab to strictly outpatient services, Darla’s intuition and professional experience led her to choose an inpatient option: Providence St. Luke’s Rehabilitation Medical Center.
The benefits and opportunities of inpatient rehabilitation
“Inpatient rehab is very multidisciplinary and team-based. It’s focused, integrated care,” she said. “Every day, from the day you arrive, you get three hours of intense therapy, which research shows is the best thing following a stroke.”

This daily therapy put Darla with a wide range of specialists, starting with her rehabilitation nurse and her physiatrist, Dr. Frank Jackson, but also including physical therapists, occupational therapists, respiratory therapists, speech therapists, neuropsychologists, and dieticians. By design, these specialists all collaborate on each patient’s care, and meet regularly—along with case managers and social workers—to coordinate care and share insights on the patient’s progress.
“It’s all related—how their medical status is presenting an inability to function in certain ways, how that lack of function might affect their mood, how their mood affects their appetite, and so on,” said Dr. Jackson. “We draw it all together so we can get the best outcomes possible for each patient.”
In Darla’s case, therapy involved working with many of the purpose-built features that distinguish the St. Luke’s facility. There’s a whole apartment on site where she could practice getting out of a regular (non-hospital) bed, using household kitchen and bathroom facilities, and getting up from a chair—or the floor.
“I’ve had three falls since I left St. Luke’s,” Darla said. “They weren’t too bad, but the last one was in the middle of the night, and I was able to do exactly what James, my physical therapist, told me. I pushed up with my feet and got up without a problem.”
In addition to the model apartment, the facility also includes:
- Cars and a portion of a bus for practicing getting in and out of motor vehicles
- A portion of a commercial passenger plane for practicing air travel
- A mock grocery store for practicing everyday shopping
- An outdoor terrain park for practicing curbs and walking on grass
- Advanced technologies for offloading patient weight to practice walking more safely
- Guidance for family members to prepare for the patient’s return to a home environment
“We tell folks this is the boot camp of getting better,” says Dr. Alicia Hegie, the St. Luke’s neuropsychologist assigned to Darla’s case. “One day at St. Luke’s is the equivalent of a week of therapy when they transition to outpatient services.”
Integrated care: The whole is greater than the sum of its parts
Because all care was coordinated, Darla benefitted from daily interaction with experts in all aspects of her recovery, in addition to the 24-hour physician support the facility provides. This circle of care forms a strong bond around the individual patient, empowering them with knowledge and motivating them to keep improving their abilities.
“The integrated care model was one of my motivations for specializing in physiatry,” said Dr. Jackson. “I’m inspired by the idea of working with an amazing team of professionals in an inpatient environment, all revolving around each individual patient’s specific needs.”
As for Darla, who continues making progress and has relocated to Spokane to live near her daughter and closer to St. Lukes, the care she received was a blessing that made her reflect in a new way on her past, long career.
“I helped a lot of people like me over those 46 years, but it was so different seeing it from their perspective,” she says. “And yet my experience really brought me comfort, too. When I first arrived in that wheelchair to St. Lukes, and I saw all those people ready to help me—it felt like I was home.”
Learn more about the stroke program at Providence St. Luke’s Rehabilitation Medical Center by visiting our website: https://www.providence.org/locations/wa/st-lukes/stroke-program
Contributing caregivers
Frank K. Jackson, DO is a physiatrist and Medical Director of the Brain Injury Program at Providence St. Luke’s Physiatry Practice in Spokane, Wash.
Alicia F. Hegie, Psy.D. is a neuropsychologist at Providence St. Luke’s Physiatry Practice in Spokane, Wash.